How Telepharmacy & E-Prescriptions Can Close Medication Access Gaps in Peri-Urban Areas
A practical, Africa-tailored guide showing how telepharmacy and e-prescription systems can shrink medication access gaps in peri-urban areas. Covers service models (hub-and-spoke, e-pharmacy, drone/SMS last-mile), regulatory checkpoints, e-prescription workflows, technology and payment options (mobile money), procurement tips, business cases, and an implementation roadmap. Includes real African examples, cheeky anecdotes, and APA references with live links.
Short brief: Peri-urban areas sit awkwardly between city pharmacies and rural clinics — too far for quick refills, too small for big-chain distribution. Telepharmacy plus e-prescriptions can plug that gap: remote pharmacist consultation, fast e-scripts, and smart last-mile delivery (courier, motorbike, drones, or CHW pickup). This guide gives hospital managers, pharmacists, health programme leads and founders a step-by-step playbook you can start using today — with the legal, technical and human bits you’ll actually need.
Expect: rib-cracking anecdotes, realistic peri-urban scenarios, an actionable 10-point checklist, vendor/use-case examples from Africa, and APA citations with live links so you can paste into proposals.
Why telepharmacy + e-prescriptions are a peri-urban superpower (short)
Peri-urban residents face frequent stockouts at local shops, inconsistent opening hours, and transport costs that make a simple refill into a half-day expedition. Telepharmacy (remote pharmacist services) combined with secure e-prescriptions and efficient delivery reduces travel, speeds access, and improves adherence — if implemented with strong workflows, regulation awareness, and local delivery options. A growing body of evidence and WHO digital-health guidance supports telemedicine interventions when they’re integrated into health systems and accompanied by governance. World Health Organization+1
Opening anecdote (for the faint-hearted)
“Mrs. Achieng finished her anti-hypertensive pills on a Sunday. The nearest pharmacy that had stock was two boda rides away and closed by dusk. She called the clinic, the nurse said ‘come tomorrow,’ and the pills weren’t taken. Two days later she called the clinic again — this time a telepharmacist answered, checked her e-prescription, and arranged a motorbike courier. Mrs. Achieng stayed out of hospital. Nobody wrote a press release — just fewer missed doses and a relieved daughter.”
Telepharmacy isn’t glamorous — it’s quietly lifesaving when it stops simple access barriers from becoming complications.
What is telepharmacy and how e-prescriptions fit in?
-
Telepharmacy: pharmacist-delivered services at a distance — counselling, medication reconciliation, prescription verification, medication therapy management, and remote adverse-event monitoring — delivered by phone, video, chat, or asynchronous platforms. PMC
-
E-prescription (e-script): a secure, electronic prescription issued by an authorized prescriber and delivered digitally to a pharmacy or e-pharmacy for verification and dispensing. E-prescriptions remove illegible handwriting, speed verification, and can be routed directly to the closest dispensing point.
When linked, telepharmacy + e-prescriptions create a workflow: clinician issues e-script → pharmacist verifies remotely → logisticians/CHWs deliver or patient picks up → pharmacist follows up for adherence/AE reporting.
10-Point Operational Checklist: What to get right before you go live
-
Regulatory compliance: confirm national rules for telepharmacy, e-prescriptions, and online pharmacies (example: Kenya’s Internet Pharmacy Guidelines). Pharmacy Board Kenya
-
Prescriber authentication: enforce digital authentication for prescribers (licensed IDs, 2FA).
-
Pharmacist verification workflow: every e-script must be reviewed by a licensed pharmacist (documented and auditable). PMC
-
Secure e-prescription format: signed, timestamped, tamper-evident records (PDF with digital signature or secure API).
-
Local dispensing network: map nearby brick-and-mortar pharmacies, kiosks, CHW hubs, couriers, or drone/last-mile partners. Zipline and similar models show that novel logistics can scale access. Zipline+1
-
Payment & affordability: mobile money integration (M-Pesa, MTN MoMo, Airtel Money) or voucher models for subsidy recipients.
-
Cold chain & special meds: identify medicines requiring cold chain or regulatory approvals (vaccines, biologics) and reserve those for qualified channels.
-
Pharmacovigilance & follow-up: rapid AE reporting and remote counselling protocols; route serious events to referral clinics.
-
Data protection & consent: follow national data laws and WHO digital health guidance — collect minimal data and document consent. World Health Organization
-
Sustainability model: clear revenue mix — patient fees, insurance reimbursement, tender/NGO contracts, or public procurement.
Proven service models you can adopt (pick your fit)
1) Hub-and-Spoke (clinic + local pharmacy)
Clinician at clinic issues e-script that routes to the nearest partner pharmacy (spoke). Pharmacist verifies remotely, then either dispenses for patient pickup or sends courier. Works well for chronic meds and peri-urban settings with many small outlets.
2) e-Pharmacy marketplace (central fulfilment + local lockers / couriers)
Central inventory and call-centre pharmacists (example: MyDawa in Kenya) receive e-scripts and dispatch orders via motorbike courier or pharmacy lockers. Useful when central inventory is more reliable than many small shops. MyDawa and similar e-pharmacies have built reputation and regulatory compliance to serve large urban and peri-urban populations. MYDAWA Blog
3) CHW-mediated telepharmacy (shared devices/hub)
CHW visits patient, connects to remote pharmacist via tablet/phone, collects e-script, and either supplies meds from CHW hub (shared stock) or requests delivery. This model reduces per-patient device costs and reaches low-tech users.
4) Drone / on-demand delivery integration
For hard-to-reach peri-urban pockets or urgent meds, integrate last-mile drone providers (where available) or rapid motorbike couriers. Zipline’s partnerships in several African countries show drones can be integrated into national supply chains for essential medicines. Zipline+1
Regulatory & safety checklist (country examples & links)
Telepharmacy sits at the intersection of pharmaceutical regulation, telemedicine rules, and data law. Before launching:
-
Check national pharmacy board guidelines for internet pharmacy/telepharmacy (e.g., Pharmacy & Poisons Board — Kenya; other national regulators publish similar rules). Verify whether e-prescriptions are permitted and what records are required. Pharmacy Board Kenya+1
-
Prescriber & pharmacist licensing: confirm remote pharmacists and prescribers are licensed in the jurisdiction of dispensing.
-
Controlled medicines: many countries restrict electronic dispensing of controlled substances — build exceptions and secure workflows.
-
Record keeping & audit: maintain auditable logs of verification, dispensing, counselling, and delivery receipts.
-
Cross-border rules: if your model uses regional warehouses, check import/export medicine regulations and registration status.
Helpful starting points: WHO consolidated telemedicine guidance and national internet pharmacy guidelines. World Health Organization+1
Technology stack — simple and robust (don’t overbuild)
-
E-prescription engine: lightweight web app or API that generates signed prescriptions.
-
Pharmacist verification portal: dashboard for remote review, notes, and approval.
-
Inventory & routing module: matches e-script to nearest dispenser with stock and flags substitutions.
-
Payments gateway: integrate major mobile-money providers; support cash-on-delivery where necessary.
-
Delivery tracking: SMS/WhatsApp updates + simple proof-of-delivery (photo or OTP).
-
EMR/PHIS integration: optional DHIS2/OpenMRS hooks for reporting and surveillance.
-
Security: TLS, role-based access, audit logs, and encrypted backups.
Start with off-the-shelf e-pharmacy platforms or customize open-source stacks; avoid bespoke enterprise systems for your first pilot.
Financing & business models that work in peri-urban settings
-
Fee-per-dispense + telepharmacy surcharge: patient pays medicine + small delivery & counselling fee.
-
Subscription for chronic care: monthly fee for medicine delivery, refill reminders, and pharmacist check-ins.
-
B2B (employers/insurers): employers or micro-insurers buy subscription services for employees.
-
Public contracting / NGO tenders: provide telepharmacy to subsidised patients under MOH/NGO agreements.
-
Hybrid donor + commercial: pilots funded by grants transition to paid services for sustainability.
e-pharmacies like MyDawa initially used mixed models (consumer sales + B2B) to strengthen unit economics and scale. MYDAWA Blog
Three African mini case studies (real / illustrative)
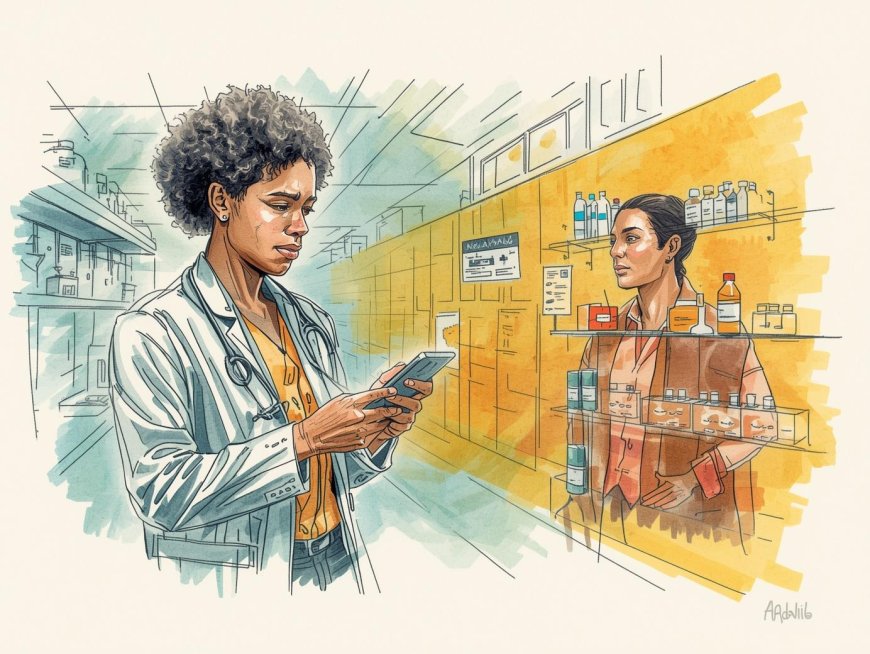
1) MyDawa — e-pharmacy & trust building (Kenya)
MyDawa built a central e-pharmacy with licensed pharmacists, digital prescriptions, and last-mile courier delivery. Earned legitimacy via certifications and a clear pharmacist verification process, showing demand for trustworthy e-pharmacy services in peri-urban and urban markets. MYDAWA Blog
2) Zipline — integrating logistics into health systems (Ghana, Rwanda, Nigeria)
Zipline’s drone network has delivered vaccines, blood, and essential medicines on national contracts — demonstrating how novel logistics can be integrated to reduce stockout and speed delivery to non-urban clinics. For peri-urban spots with bad roads, such services can be a game changer when combined with telepharmacy verification. Zipline+1
3) Telepharmacy evidence base (systematic reviews)
Systematic reviews and region-level studies indicate telepharmacy can improve access, adherence and counselling reach in rural/underserved settings — but adoption barriers include regulation, digital skills, and infrastructure; implementation must be context-sensitive. PMC+1
Common pitfalls (and how to dodge them)
-
Pitfall: Launching without regulatory checks → Fix: get written confirmation from national pharmacy board on e-prescription acceptance and record requirements. Pharmacy Board Kenya
-
Pitfall: No pharmacist verification → Fix: every e-script must be approved by a licensed pharmacist before dispensing. PMC
-
Pitfall: Ignoring cold-chain or controlled medicines → Fix: route those meds through validated supply chains only.
-
Pitfall: No affordable delivery → Fix: negotiate bulk courier rates, use CHW hubs, or explore drone partners where feasible. Zipline
-
Pitfall: Poor patient data protection → Fix: implement consent, minimal data retention, and encrypted records. World Health Organization
Ready-to-use 8-week implementation roadmap (pilot for a peri-urban subcounty)
Week 0–1 — Stakeholder & legal check
-
Meet pharmacy board and MOH for guidance and approvals. Map local pharmacies and logistics partners. Pharmacy Board Kenya
Week 2–3 — Build minimal tech & workflows
-
Set up e-prescription portal, pharmacist verification dashboard, delivery routing (simple courier list), and mobile-money integration.
Week 4 — Train staff & pharmacies
-
Train clinicians to issue e-scripts, pharmacists on verification SOP, and couriers on proof-of-delivery.
Week 5–6 — Soft launch (100 patients)
-
Start with controlled chronic meds (hypertension, diabetes); use CHW hubs for patients without phones.
Week 7 — Monitor & iterate
-
Track delivery times, verification times, patient satisfaction, adverse events, and regulatory feedback.
Week 8 — Scale to 500 patients
-
Expand geographically and consider adding subscription options or insurer partnerships.
Quick SOP snippet for pharmacist verification (pin at the counter)
-
Receive e-script request (app/web) → timestamped.
-
Confirm prescriber identity and license.
-
Check medication name, dose, contraindications, and interactions.
-
Document verification and counselling notes.
-
Allocate stock or dispatch courier.
-
Send SMS/WhatsApp confirmation with expected delivery time and a short safety message.
-
Log proof-of-delivery and follow up for AE within 72 hours.
Final one-page checklist to copy into your procurement email
-
Regulatory check with Pharmacy Board done? (link to written guidance). Pharmacy Board Kenya
-
Prescriber authentication method defined? Y/N.
-
Pharmacist verification workflow documented? Y/N. PMC
-
Local dispensing partners mapped? Y/N.
-
Delivery partner (courier/drone/CHW) contracted? Y/N. Zipline
-
Mobile money payment integrated? Y/N.
-
Data protection & consent scripts ready? Y/N. World Health Organization
-
Pilot budget & timeframe approved? Y/N.
References (APA — live links)
-
World Health Organization. (2022). Consolidated telemedicine implementation guide. https://www.who.int/publications/i/item/9789240059184. World Health Organization
-
Nwachukwu, C. A., et al. (2023). Effectiveness of Telepharmacy in Rural Communities: A Systematic Review. Journal / PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC10515969/. PMC
-
Hedima, E. W., et al. (2020). Telepharmacy: An opportunity for community pharmacists. Journal / PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC7609244/. PMC
-
Pharmacy and Poisons Board (Kenya). (2022). Guidelines for Internet Pharmacy Services in Kenya. https://web.pharmacyboardkenya.org/download/guidelines-on-internet-pharmacy-services/. Pharmacy Board Kenya
-
Zipline. (n.d.). Africa — Drone delivery & logistics for public health. https://www.zipline.com/africa. Zipline
-
MyDawa. (2019). MyDawa becomes first e-pharmacy in Africa to earn LegitScript certification. https://blog.mydawa.com/mydawa-becomes-first-e-pharmacy-in-africa-to-earn-legitscript-certification/. MYDAWA Blog
-
Jairoun, A. A., et al. (2025). The evolution of medication delivery via drones. MDPI / PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC12210395/. PMC
-
Mekurianew Kelkay, J., et al. (2024). Adoption of telepharmacy among pharmacists, physicians and nurses in Hawassa public hospitals, Ethiopia. PLOS Digital Health. https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000693. PLOS
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0