Remote monitoring on a budget: Affordable device combos for chronic care
A pragmatic, Africa-focused guide to setting up low-cost remote patient monitoring (RPM) for chronic conditions (hypertension, diabetes, heart failure, COPD). Covers affordable device combos, connectivity and power hacks, clinical workflows, procurement tips, validation needs, pitfalls, and a ready-to-use checklist — with evidence-backed citations and live links. Ideal for district hospitals, NGOs, CHW programmes and small private clinics.
Short brief: Want to keep patients with hypertension, diabetes or heart failure safely at home — without burning your budget on expensive IoT stacks? This is your playbook. Practical device combos, real-world deployment tips (solar chargers! shared hubs!), safety/accuracy caveats, and procurement checklists — all written with an African clinic’s realities in mind (power cuts, patchy networks, shared phones, and busy nurses who want things that simply work).
Expect rib-cracking field anecdotes, one realistic case vignette, and APA-style references with live links so you can paste into proposals.
Why RPM (remotely) — and why “budget” matters
Remote monitoring can reduce clinic visits, detect early deterioration, and keep medication adherence on track for chronic patients. Systematic reviews show RPM can improve some clinical outcomes and reduce readmissions in chronic conditions when combined with clinical follow-up — but benefits depend on device accuracy, clinical pathways, and reliable data flows. If you design for local constraints — low bandwidth, intermittent power, and shared devices — RPM can be affordable and effective. Nature+1
Quick rib-cracker to start: “The Band-Aid that rang”
A rural clinic bought fanciest pulse oximeters, set up SMS alerts — and the nurse got five alarms at 2 AM from patients who’d read the device incorrectly. After a week they switched to training + a finger oximeter with a one-page pictorial guide and routed urgent alarms to the on-call clinician rather than automatic SMS blasts. The moral: cheaper plus training > shiny gadget alone.
Which affordable device combos actually work? (by clinical scenario)
Below are practical, low-cost bundles you can mix-and-match depending on the condition you’re monitoring. Each combo prioritizes clinical value, simplicity, and cost-effectiveness.
1 — Hypertension monitoring (most common, most bang for buck)
-
Core devices: Upper-arm validated automated BP cuff (digital, oscillometric) + basic weight scale (optional).
-
Connectivity options: Bluetooth cuff to patient smartphone (if available) OR shared clinic/CHW tablet with Bluetooth; manual SMS reporting via CHW if no smartphone.
-
Why this combo: Home BP monitoring with validated upper-arm cuffs improves BP control versus usual care when readings are used in decision-making. Choose validated devices (see validation lists) — wrist cuffs and unvalidated brands are riskier. JMIR Publications+1
Affordable picks & notes: Many models from OMRON and similar brands are widely available and have validation studies; low-cost generic upper-arm cuffs under $30–$60 may work but insist on validation documentation. Avoid wrist cuffs for clinic workflows. (See device validation guidance below.) JMIR Publications
2 — Diabetes (remote glucose monitoring)
-
Core devices: Strip-based glucometer + test strips (patient pays per-test) OR connected glucometer for insulin-dependent patients.
-
Connectivity: Patient reads and sends SMS/USSD with reading, or CHW uploads readings during weekly visits. For insulin users, consider Bluetooth-capable glucometers that sync to apps.
-
Why this combo: Self-monitoring of blood glucose (SMBG) supports medication titration and hypoglycaemia detection; affordability is driven by ongoing strip cost. Budget for strips first. PMC
Procurement tip: Buy meters with inexpensive, locally-available strips; negotiate bulk strip pricing with suppliers or partners. Validate strip supply chain before scaling.
3 — Heart failure & fluid-sensitive patients
-
Core devices: Digital weighing scale (accurate to 100 g if possible) + automated BP cuff + symptom checklist via SMS/IVR. Optionally pulse oximeter if respiratory symptoms are common.
-
Workflow: Daily/alternate-day weight logs (home or CHW-measured) trigger nurse review for >2 kg gain over 48–72 hours. Clinician phone triage and early diuretic adjustment avert admissions. Evidence shows weight and symptom telemonitoring can help when connected to actionable clinical pathways. JMIR Publications+1
4 — COPD / chronic respiratory disease (oxygen risk)
-
Core devices: Fingertip pulse oximeter (validated) + symptom diary (SMS/IVR) + inhaler adherence check-ins.
-
Caveat on pulse oximeters: Low-cost oximeters are useful for trend detection but have accuracy limitations (especially at lower saturations and in darker skin tones); use them as trend tools and combine with symptoms/clinical review. The FDA and recent reviews highlight accuracy and equity concerns — pick higher-quality clinical-grade oximeters when possible and perform local spot-check validation. U.S. Food and Drug Administration+1
How to pick devices: a short checklist (don’t buy blind)
-
Clinical validation / accuracy evidence — look for independent validation studies or listing on device validation registries. If no external data, plan local spot validation. JMIR Publications+1
-
Ease of use — single-button operation, clear displays, pictorial manuals in local language.
-
Battery & charging — long battery life; USB-C charging preferred; budget for solar banks where grid is unreliable.
-
Connectivity — Bluetooth for smartphones; otherwise ability to export results via USB or use CHW tablet. Simpler is better.
-
Consumables cost (glucometer strips, calibration) — compute ongoing cost before pilots.
-
Durability / IP rating — dust and humidity protection matter.
-
Regulatory status — national regulator registration (if used clinically) or at least supplier documentation.
-
Equity & bias checks — especially for pulse oximeters: check performance across skin tones where possible. U.S. Food and Drug Administration+1
Data & connectivity on a shoestring
Low-data workflows that work
-
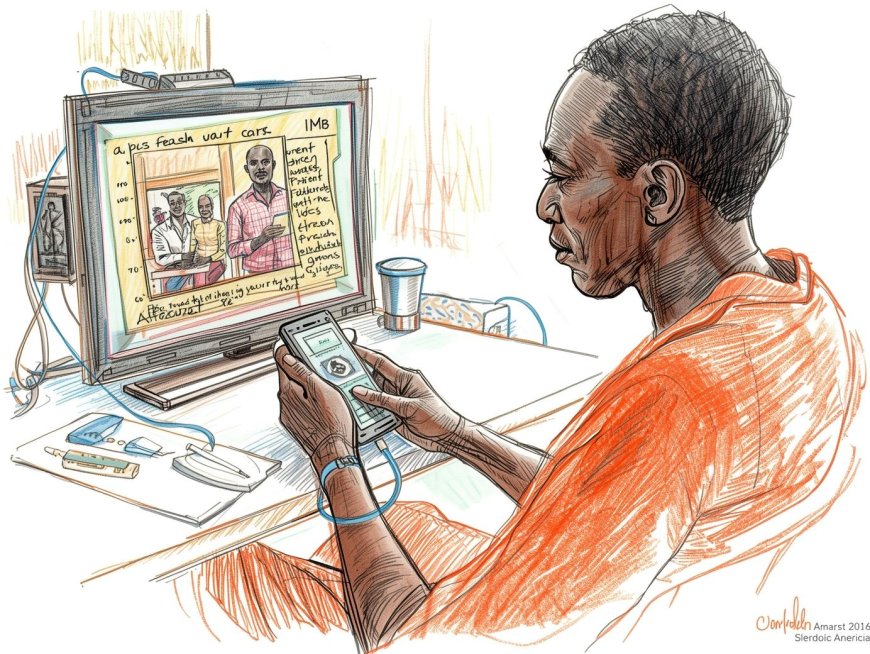
Human-in-the-loop SMS: patient texts key readings (BP/glucose/weight) in a simple format (e.g., BP 132/82). CHW or nurse parses and acts. Low tech, low cost, robust. (Use keyword parsers.) PMC
-
Shared CHW tablet hubs: CHW collects readings during weekly home visits and uploads when they hit clinic Wi-Fi. This centralises devices (fewer per-patient devices) and reduces per-patient hardware costs. PMC
-
Bluetooth → patient phone → SMS gateway: where smartphone prevalence is adequate, a Bluetooth cuff/glucometer syncs to a simple app that then compresses and sends batched data via mobile internet or SMS gateway.
Power & charging hacks
-
Solar power banks for devices and phones (budget 10–20 USD per unit as a starter). Rugged USB-C chargers, magnetic pogo-pin cradles for easier use, and a battery-inverter at the clinic (UPS) for hubs. These small investments prevent most dropout due to “phone dead” or “device dead” problems.
Clinical workflow design — keep it simple and safe
-
Define thresholds & actions before deployment (e.g., BP >160/100 = urgent call within 4 hours; weight gain >2kg in 48 hrs = nurse review).
-
Triage routing: automatic flags (SMS keyword or dashboard) go to a nurse, who calls patient and documents action. Avoid auto-prescribing by algorithm unless tightly regulated and validated. World Health Organization
-
Documentation: store readings in simple CSV/EMR modules that can export to DHIS2/OpenMRS for reporting. World Health Organization
-
Patient education: include pictorial one-pagers on how to measure BP, how to place the pulse oximeter, and when to call. Training reduces false alarms.
Validation — don’t trust factory claims
-
Spot-checks: Validate a sample of devices against clinic-grade devices (10–30 patients) before scale-up. For BP, use clinic sphygmomanometer or validated automatic device as reference. For oximeters, follow local verification protocols and be aware of skin-tone biases flagged by regulators. U.S. Food and Drug Administration+1
-
Usability testing: watch patients perform measurements; fix common errors (wrong cuff size, low battery, nail polish on oximeters, cold fingers).
Procurement tips & money-saving hacks
-
Buy validated, not cheapest — an inexpensive unvalidated device may cost lives and money later.
-
Negotiate strip/device bundles with suppliers for glucometer strips to reduce per-test cost.
-
Shared-device model — CHW hubs or clinic-loans reduce per-patient hardware spending while preserving monitoring coverage.
-
Local suppliers & service — prioritize vendors that can provide spare parts and local warranty service.
-
Plan total cost of ownership (TCO) for 12–24 months: devices, consumables, training, power gear, data costs, and local support. PMC
One short real-ish case vignette
Kisumu County RPM Pilot (hypothetical, realistic)
Kisumu County ran a 6-month pilot for 200 patients with hypertension and 50 heart-failure patients. They used an OMRON-validated upper-arm cuff (clinic loan model), a simple digital scale at CHW hubs, and SMS check-ins. CHWs visited patients weekly to sync readings (tablet hub) and were trained to call clinicians for red flags. Result: median systolic BP fell by 8 mmHg among engaged patients; two early decompensations were caught and treated at home, avoiding admission. Success drivers: validated BP cuffs, CHW hubs, clear escalation thresholds, and solar power banks. (This approach is supported by RPM and telemonitoring evidence when combined with clinical follow-up.) Nature+1
Common pitfalls (and quick fixes)
-
Pitfall: Buying unvalidated cheap devices. → Fix: Require validation papers; do spot checks. JMIR Publications
-
Pitfall: Relying on pulse oximetry alone for decisions. → Fix: Use oximeters as one input among symptoms and clinician review; be aware of accuracy limitations in darker skin. U.S. Food and Drug Administration+1
-
Pitfall: No human triage. → Fix: Route alerts to clinicians/CHWs; don’t let algorithms act alone. World Health Organization
-
Pitfall: Under-budgeting consumables (glucometer strips). → Fix: Calculate per-patient strip costs and fund them before scale.
Budget-friendly RPM deployment checklist (copy-paste)
-
Clinical target & thresholds defined (BP/glucose/weight/SpO₂).
-
Device list with validation evidence saved.
-
CHW hub / shared-device model considered (Y/N).
-
Data pathway mapped (SMS / tablet / smartphone app).
-
Power plan (solar banks / clinic UPS) budgeted.
-
Consumables budgeted (strips, batteries).
-
Training plan & pictorial job-aids created.
-
Triage/escalation SOP written and tested.
-
Spot-validation plan for devices (n=20–30) scheduled.
-
Local supplier & warranty confirmed.
Further reading & APA references (live links)
-
Tan, S. Y., et al. (2024). A systematic review of the impacts of remote patient monitoring interventions. NPJ Digital Medicine. https://www.nature.com/articles/s41746-024-01182-w. Nature
-
Peyroteo, M., et al. (2021). Remote Monitoring Systems for Patients With Chronic Diseases: Systematic Review. JMIR. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8734917/. PMC
-
World Health Organization. (2019). Recommendations on digital interventions for health system strengthening. https://www.who.int/publications/i/item/9789241550505. World Health Organization
-
Stevenson, L. W. (2023). Remote Monitoring for Heart Failure Management at Home. Journal of the American College of Cardiology. https://www.jacc.org/doi/10.1016/j.jacc.2023.04.010. JACC
-
Rojas, A. N., et al. (2024). Advances and Challenges Associated with Low-Cost Pulse Oximeters. Sensors (MDPI). https://www.mdpi.com/1424-8220/24/19/6284. MDPI
-
Nemomssa, H. D., et al. (2022). Development of Low-Cost and Portable Pulse Oximeter. Scientific Reports / related open paper. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9084508/. PMC
-
U.S. Food and Drug Administration. (2024). Performance Evaluation of Pulse Oximeters (Executive Summary). https://www.fda.gov/media/175828/download. U.S. Food and Drug Administration
-
Ding, H., et al. (2020). Effects of Different Telemonitoring Strategies on Chronic Disease Outcomes: Systematic Review. JMIR. https://www.jmir.org/2020/11/e20032/. JMIR Publications
-
World Health Organization. (n.d.). Digital health topics and tools. https://www.who.int/health-topics/digital-health. World Health Organization
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0